by ICWA
What are your chances of transmitting SARS-CoV-2 if you tested positive?
On December 14, 2020, JAMA Network Open published a paper titled “Household Transmission of SARS-CoV-2, Systematic Review and Meta-analysis.” The authors have analyzed the data from relevant studies to estimate the rates of transmission of SARS-CoV-2 from index (primary) cases to secondary contacts within their households. According to their findings, whenever index cases were sick (symptomatic), the household secondary attack rate was 18%. However, when index cases were not sick (asymptomatic) at the time of contact, the rate of transmission to household members or relatives was only 0.7%.
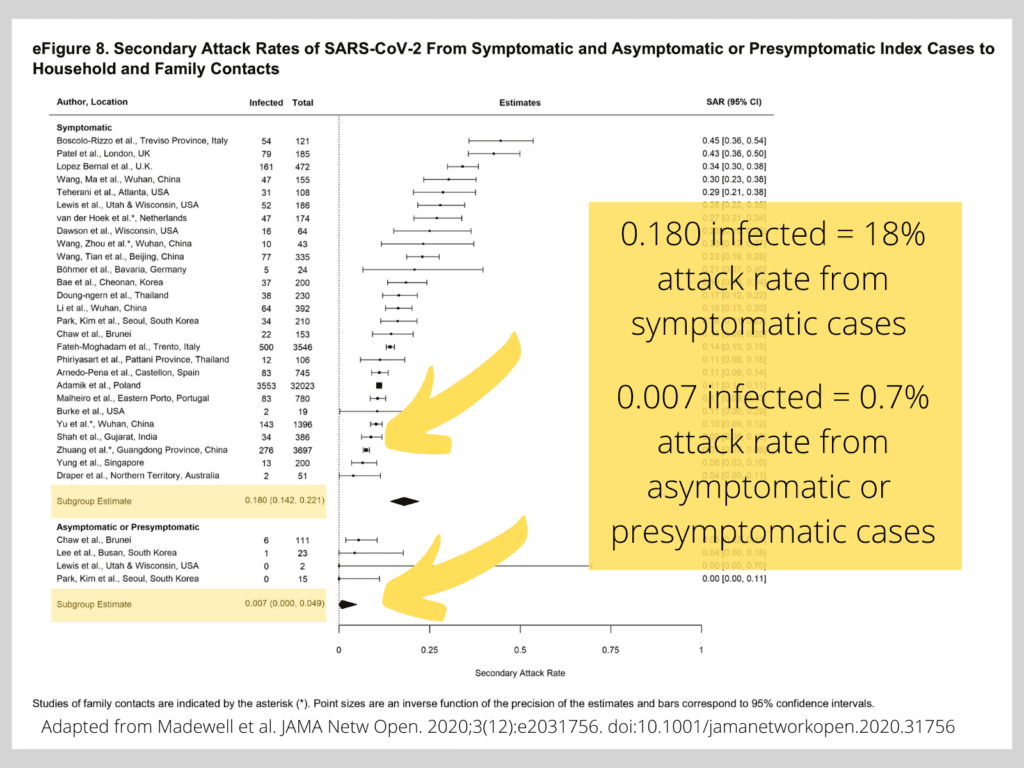
People without symptoms at the time of testing can be either pre-symptomatic (those who will develop disease symptoms in a few days) or asymptomatic carriers (those who never develop any symptoms despite testing positive for the virus). In eAppendix 4. Additional Description of Risk Factors, the authors of the Systematic Review cite a study that further shows the difference between these two types of asymptomatic people: “Another [study] reported a higher secondary attack rate among close contacts of pre-symptomatic index cases than asymptomatic carriers.13”
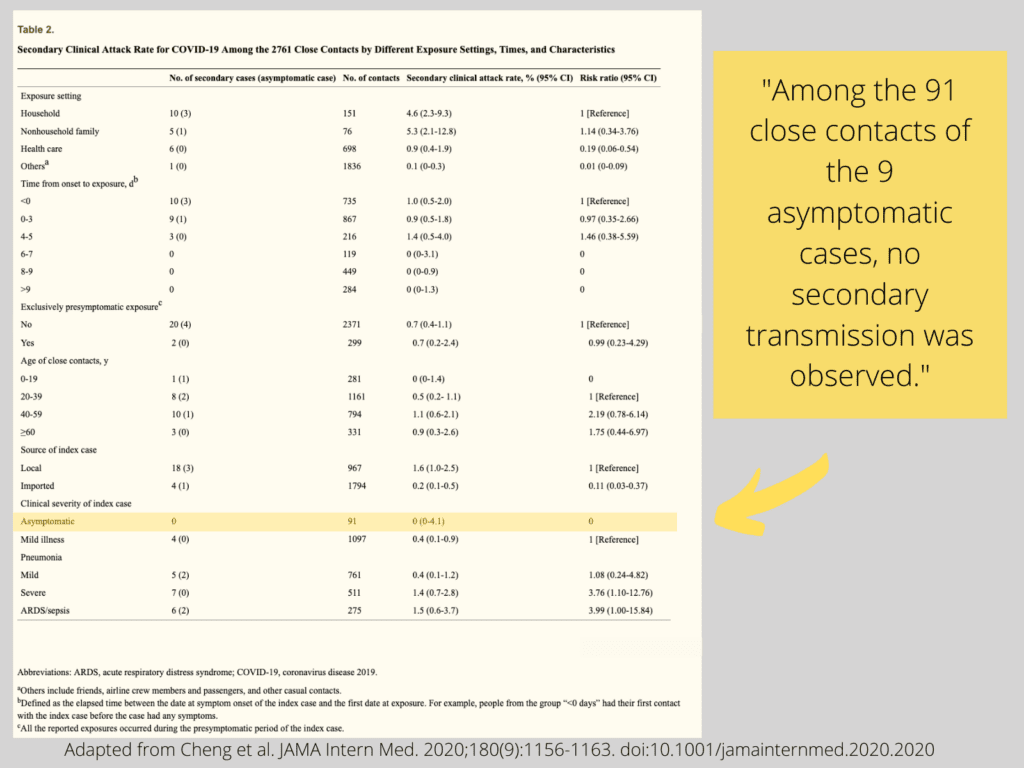
Their reference #13 brings up a study published on May 1, 2020 in JAMA Internal Medicine titled “Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan and Risk at Different Exposure Periods Before and After Symptom Onset.” Here, the authors state the following: “The 299 contacts with exclusive pre-symptomatic exposures were… at risk (attack rate, 0.7% [95% CI, 0.2%-2.4%]).” In contrast, with respect to bona fide asymptomatic carriers, they state: “Among the 91 close contacts of the 9 asymptomatic cases, no secondary transmission was observed.”
So, a ‘higher’ secondary attack rate among close contacts of pre-symptomatic index cases compared to fully asymptomatic carriers amounts to 0.7% vs. nil.
In other words, those who tested positive but never developed the symptoms of COVID-19 had not been found to infect others, while the chances of pre-symptomatic persons to infect others were rather low compared to those who were actually sick at the time of contact.
Why does a positive PCR test not always mean you are sick or even contagious?
Currently, a nucleic acid amplification test called Polymerase Chain Reaction (PCR) is being used to identify those who may have the virus.
Even though PCR is a Nobel Prize-winning methodology that has greatly advanced the field of Molecular Biology, the manner in which it has been (mis)used by public health authorities in detecting the presence of the SARS-CoV-2 virus has drawn severe criticism from the scientific community. An international group of scientists even demanded a retraction of the test due to numerous methodological and molecular design flaws.
“In light of our re-examination of the test protocol to identify SARS-CoV-2 described in the Corman-Drosten paper we have identified concerning errors and inherent fallacies which render the SARS-CoV-2 PCR test useless.“
https://cormandrostenreview.com/report/
Because all that a PCR test can do is amplify genetic material, to utilize it as a correlate of a bona fide viral infection, it needs to be validated against a test that actually detects an infectious (cultivable) virus. Only then can it be used as a valid correlate and more faithfully represent the presence of an infectious virus in a patient’s sample.
A French group of researchers did just that: they tested PCR-positive samples against viral cultivability of SARS-CoV-2. Their recent study, published in Clinical Infectious Diseases, shows that there’s a fairly good correlation between PCR positivity and viral cultivability at PCR cycle thresholds (Ct) of under 25 cycles. At Ct > 35, however, the correspondence rate is a mere 2.7% or less.
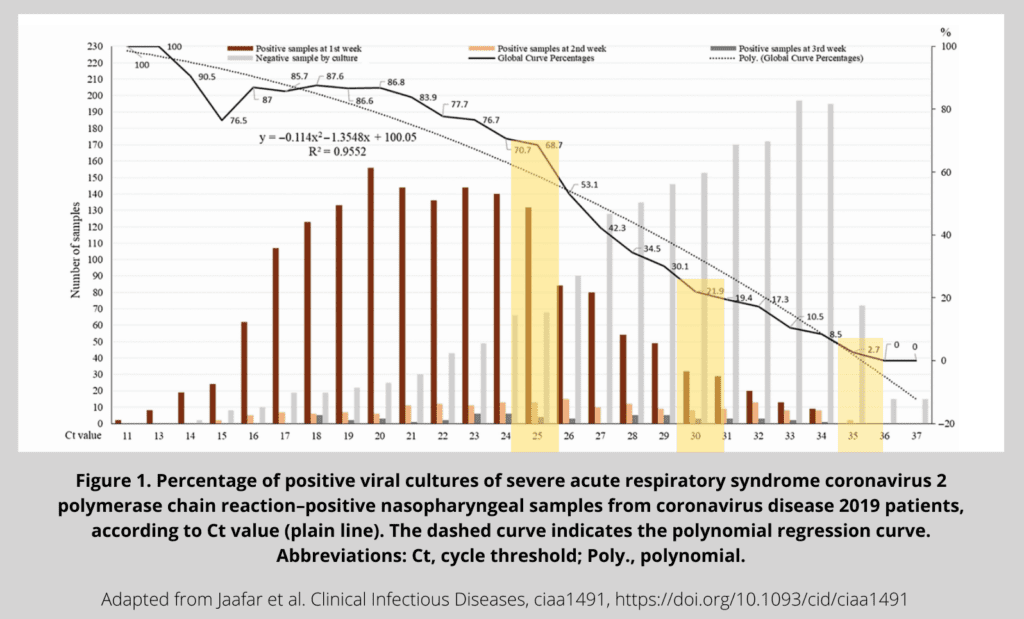
It is also well known among molecular biologists that with too many rounds of amplification (known as “cycles”), PCR tends to produce false-positives—that is, to amplify some random junk rather than a targeted nucleic acid piece from a collected sample.
A PCR test could have been rendered useful for SARS-CoV-2 detection, as it’s a quicker and easier method than viral cultivation from each patient’s sample. But because labs continue to report positive tests to public health departments at Ct higher than 35 and do not disclose the Ct value upon which each individual PCR test turns positive, we have a situation where healthy people are being labeled as positive for a viral phantom they neither get sick from nor transmit to close contacts. And quite possibly, these individuals may not even carry the said virus. They are not a danger to themselves or to others, and yet they are considered ‘cases’ and are required to quarantine themselves. These phantom ‘cases’ likely continue to spike the perceived high incidence of COVID-19, triggering a ripple effect of restrictions, isolations, testing, and all the disruption and loss that entails.
If, instead of fanning the pandemic with over-inflated PCR testing, public health authorities had turned their efforts to developing proper methods of distinguishing between pre-symptomatic infectious cases and non-cases, we would all be better off.
If you are told your PCR test is positive,
demand to know the Ct value of your test.