What is personalized medicine?
Personalized medicine is a medical approach in which drugs, treatments, and other modalities are tailored to account for an individual’s current state of health, unique genetic and environmental factors, and lifestyle in order to maximize efficacy and minimize the risk of side effects.
Personalized medicine is not a new concept. As pointed out by Personalized Medicine Coalition:
“For more than two millennia, medicine has not wavered from its aspiration of being personalized. In ancient times, Hippocrates combined an assessment of the four humours—blood, phlegm, yellow bile, and black bile—to determine the best course of treatment for each patient.”
Nevertheless, modern medicine has attempted to apply the unsuitable principles of industrial manufacturing to the treatment of patients, with “standard of care” and “standing orders” being rigorously enforced to the detriment of the individual patient, and often tying the hands of doctors.
From “The Case for Personalized Medicine“ in 2014:
As modern medicine is slowly embracing personalization, by incorporating the latest science into products, treatments, and administration to maximize benefits and avoid unnecessary risks, should the concept of personalized medicine also be applied to vaccination?
Regulatory and science agencies as well as leading experts in vaccination recognize the importance of host-specific factors that influence immune responses and adverse reactions to vaccination.
The CDC’s Pink Book states:
“Many factors may influence the immune response to vaccination. These include the presence of maternal antibody, nature and dose of antigen, route of administration, and the presence of an adjuvant (e.g., aluminum-containing material added to improve the immunogenicity of the vaccine). Host factors such as age, nutritional factors, genetics, and coexisting disease, may also affect the response.”
The 2012 IOM (Institute of Medicine) report titled “Adverse Effects of Vaccines: Evidence and Causality” admits:
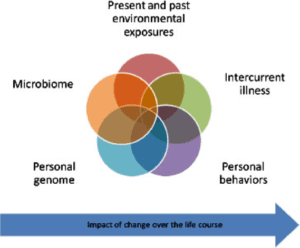
“Both epidemiologic and mechanistic research suggests that most individuals who experience an adverse reaction to vaccines have a preexisting susceptibility. These predispositions can exist for a number of reasons—genetic variants (in human or microbiome DNA), environmental exposures, behaviors, intervening illness, or developmental stage, to name just a few—all of which can interact as suggested graphically in Figure 3-1 [left]. Some of these adverse reactions are specific to the particular vaccine, while others may not be. Some of these predispositions may be detectable prior to the administration of vaccine; others, at least with current technology and practice, are not. Moreover, the occurrence of the adverse event is often the first sign of the underlying condition that confers susceptibility.”
Leading MD researchers in the field of vaccinomics and autoimmunity, such as Dr. Gregory Poland of Mayo Clinic, Rochester, MN and Dr. Yehuda Shoenfeld of Sheba Medical Center, Tel-Aviv, Israel, both support this notion:
“ . . .the idea not so much that we would make a vaccine for an individual person, but that we would begin to use age, disease state, medical condition, genomic information, and systems biology or ‘vaccinomics’ information to do several things: predict who should get a vaccine, what dose they should get in how many doses, predict whether they’re going to have a response to that vaccine, predict whether they’re at risk for the disease that we’re immunizing them for, and predict whether they’re going to have a side effect for that vaccine.” ~Dr. Gregory Poland
“ . . .the fact that vaccines are delivered to billions of people without preliminary screening for underlying susceptibilities is thus of concern. Indeed, it is naïve to believe that all humans are alike.” ~Dr. Yehuda Shoenfeld, Vaccines and Autoimmunity (2015).
And what about the new field of ‘adversomics”? Research Director of Consumer Policy Institute Lawrence Solomon explains:
“. . . the vaccine research team at Mayo Clinic — one of the world’s largest, most respected and most prolific — promotes the growing discipline of “adversomics,” which aims to understand the adverse effects that can come of vaccines. The science here is daunting, since the variables that could cause a vaccine to do harm involve “a complex interaction of past exposures and infections, current physical and emotional health, and the individual’s genome and microbiome . . . Today’s vaccines are failing. Personalized vaccines that reflect an individual’s genetic profile are coming. Traditional vaccines work on a century-old model of “Isolate, Inactivate, Inject” — the tried-but-not-always-true method of making a vaccine by isolating a pathogen, stripping it of its potency and then injecting it into us. This crude approach to developing a vaccine, reliant on observation rather than theory, becomes all the cruder by delivering it in one-size-suits-all fashion.”
It is apparent that an individualized vaccine schedule is the only ethical approach if vaccination is chosen. And due to many unknowns that still exist in modern vaccination research, a personal choice to not vaccinate must be respected as well. Public health policies that do not allow for an individualized vaccination approach or personal choice put children’s health at risk of avoidable vaccine injury.